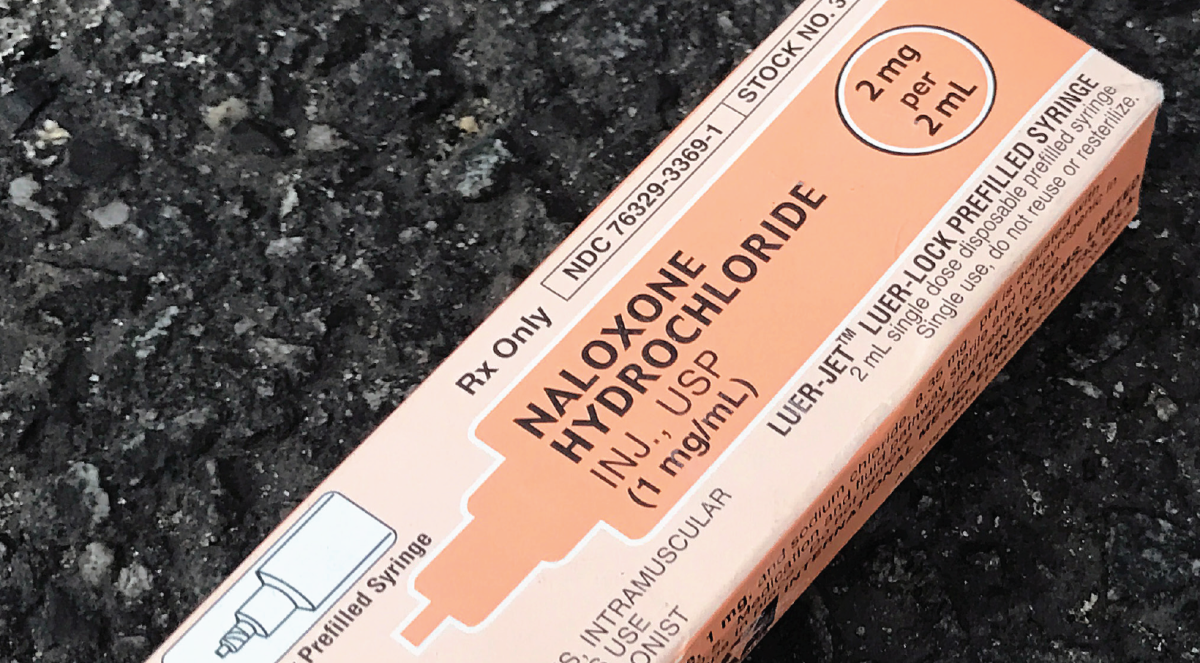
As of April 26, the city of Philadelphia had administered 1,193,155 total doses of the COVID-19 vaccine, with white individuals receiving their doses at higher rates than their Black and Hispanic counterparts, according to the latest data from the Philadelphia Department of Public Health (PDPH).
The city administered 40% of the total number of first doses to white individuals, while administering 22% to Black individuals and 23% to Hispanic individuals as of April 26, according to the PDPH.
Dr. José Torradas, the medical director of Unidos Contra COVID (United Against COVID), an “ad hoc group of Hispanic, medical professionals,” said his group is looking to address the inequities of vaccine distribution in the city’s Black and Hispanic communities.
“The disproportionality of Black and Hispanic people being affected worse from the pandemic has been set up over generations in this country,” Torradas said. “Federal, state and local policy has tended not to favor these groups.”
Philadelphia is not unique in its racial disparities of vaccine distribution. According to Dr. Rochelle Walensky, director of the Centers for Disease Control and Prevention, only 8.4% of Black individuals and only 10.7% of Hispanic or Latino individuals have received at least one dose of their vaccine in the U.S. as of April 12. Walensky recently declared racism a serious threat to public health.
Nneka Sederstrom, Ph.D., chief health equity officer with Hennepin Healthcare in Minnesota, wrote in response to written questions from The Hawk that because the country has prioritized a quick rollout plan, it has been done at the expense of equity.
“With the focus on speed and not equity, what was done continued to exacerbate problems within these communities as a result of systemic racism,” Sederstrom said. “Not intentionally calling out race as a risk factor that needed to be prioritized the distribution plan missed the mark on equity and uplifted systemic racism.”
Sederstrom said because the health care system has been built upon white supremacy and racism, the distribution of vaccines reflects this history.
Thi Nguyen ’21, a biology major and an undergraduate fellow at the St. Joe’s Institute of Clinical Bioethics, wrote in response to written questions from The Hawk that these systemic issues are highlighted in multiple ways, including technological and vocational barriers.
“Underserved communities often don’t have access to the internet,” Nguyen said. “This would make it quite difficult to obtain knowledge on vaccine efficacy, safety and clinics. Even if vaccines were available, the distribution issue would still persist if these populations were not aware of availability.”
Crystal Piñeiros ’21, also a biology major and an undergraduate fellow with the Institute of Clinical Bioethics, said these systemic issues have created an environment where, if vaccines are available, there remains hesitancy to get the shot.
“Among the Hispanic people I know in my community in New Jersey, there’s even a fear of vaccination because we’re unaware of what it contains, how can it affect us and is it really meant to benefit us,” Piñeiros said. “It’s always been us versus them with our white counterparts and it’s still a fear.”
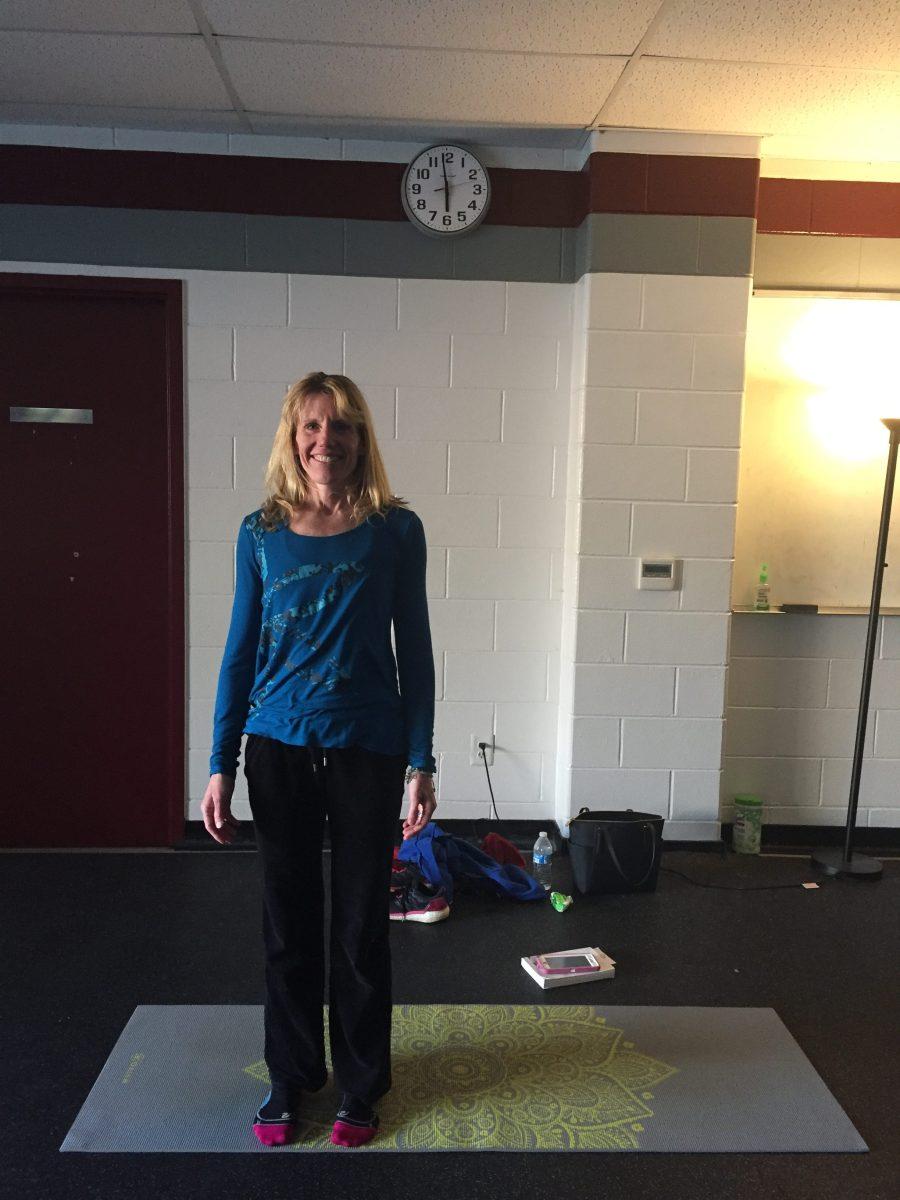
Sally Kuykendall, Ph.D., professor of health studies, chair of the Department of Health Studies and a member of the university’s vaccine working group, wrote in response to written questions from The Hawk that there are multiple possible action steps that could be taken to address these systemic issues.
“To help everyone and particularly our most vulnerable friends and neighbors, we need to invest in an educated and diverse workforce with skills in the basic sciences, data management and cultural competency,” Kuykendall said.
Torradas said Unidos Contra COVID’s efforts to pursue culturally competent care have included making connections with community leaders and local vaccine providers to create an environment of inclusivity and trust. Torradas said this will be put into action at an upcoming event with a local vaccine provider on May 2.
“We want to just reach out to the local community and basically have it staffed completely with Spanish speakers and have the reach out be Spanish speakers as well,” Torradas said. “We recognize that culturally competent care or that being able to connect with somebody linguistically may make all the difference.”
Torradas said through these local efforts and the increased attention from the government on providing the vaccine to communities of color particularly in Philadelphia, there is reason to be optimistic.
“It’s 134 square miles and 1.6 million people, 60% of whom are Black and Hispanic,” Torradas said. “So you start to put the pieces together in the city with all the things that other people are doing and that’s how we get through this.”
Nick Karpinski ’21 contributed to this reporting.