When Emily Fordham ’21, a psychology major, was diagnosed with type 1 diabetes last summer, she started wondering if she had chosen the right career path, one that would pay her medical bills.
“It isn’t the most lucrative industry,” Fordham said. “Once I wrapped my head
around what I was living with, I started asking questions like, ‘How much does this cost?’”
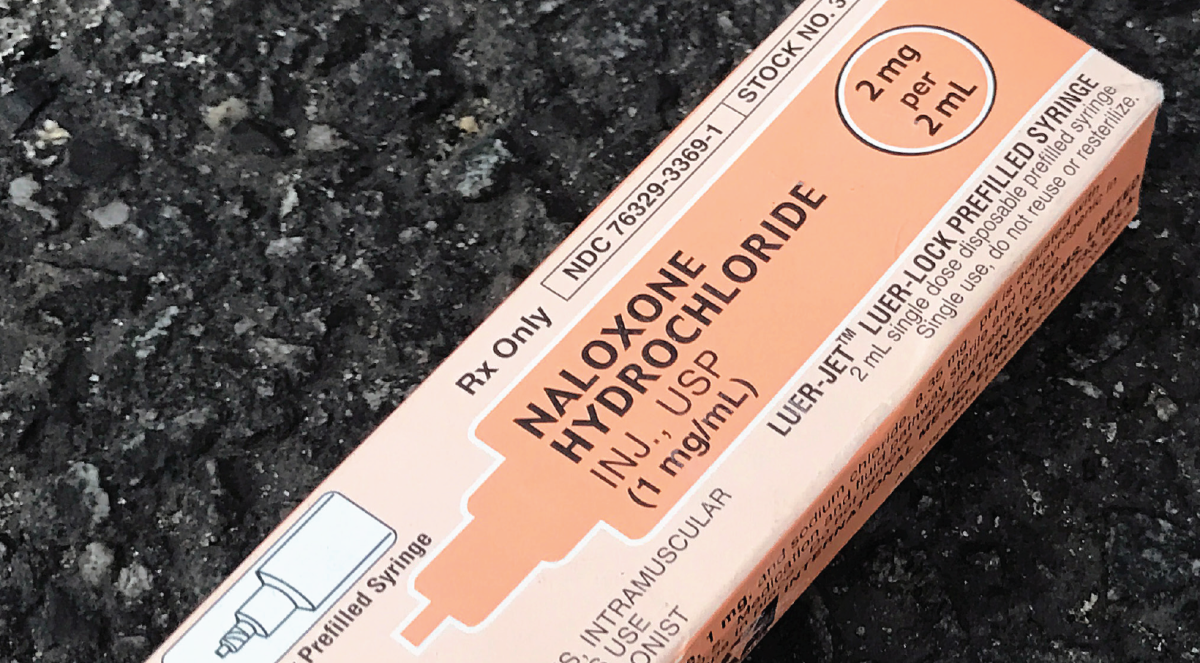
When it comes to insulin, the answer to that question can be staggering. The price of insulin has increased over 500 percent since 2005, according to a study done by the Health Care Cost Institute. In 2017, American diabetes patients paid $237 billion in direct medical costs, an average of $16,750 per patient, according to WebMD Health News.
The development of type 1 diabetes occurs when the pancreas fails to produce the insulin a person needs, making the individual dependent on injected insulin for the body to function properly. Type 2 diabetes is the body’s resistance to naturally produced insulin. In this case, changes to diet and lifestyle are often recommended before insulin treatment.
For people with diabetes, the growing cost of insulin in the last decade has led people to turn to the black market, travel abroad to buy insulin, or buy what they can afford and ration.

George Sillup, Ph.D., chair and associate professor of pharmaceutical and healthcare marketing, said insulin costs are the result of aggressive price increases by manufacturers.
“Manufacturers have adjusted their formulations to create new analogs that can extend their product’s patent protection,” Sillup said. “This extended patent protection, or ‘evergreening,’ enables the company to prevent a less expensive or generic (biosimilar) version of their products so they can continue to raise their prices without other competition.”
Sillup also blamed a lack of competition in the market. The top three manufacturers of insulin, Sanofi, Novo Nordisk and Eli Lilly and Company, continue to raise their prices, leaving those affected only one choice – to keep paying, Sillup said.
For many college students, these costs are an added worry to decisions regarding their futures.
“Everyone in college is worried about what they’re going to do after college, how
are they going to support their dreams,” Fordham said. “Then having this additional cost on top of that, it definitely factors into how you’re going to do things.”
Katherine Grimm ’21, who was diag- nosed with type 1 diabetes when she was 9 years old, pays $600 every three months for her insulin, even with insurance coverage.
“It’s incredibly frustrating to know that I have a need for this one thing, and it’s incredibly easy to make,” Grimm said. “They’ve been doing it since the 1920s. It’s just corporate greed.”
When Frederick Banting, M.D., and Charles Best, M.D., discovered insulin as a treatment for diabetes in 1921, they sold the patent to University of Toronto for $1, in hopes it would lead to affordable access for everyone who needed it. Today, because no generic versions of insulin exist and there are only four major companies controlling the market, the prices have in- creased although no substantial changes to the drug has been made.
Fordham said she is appalled that companies are profiting off her insulin dependency.
“Taking advantage of a situation someone is in to make a profit off of someone who is less fortunate and diagnosed with some- thing they did nothing to deserve,” Fordham said. It’s just not right.”
Walter Bryz-Gornia ’21, who was diagnosed with type 1 diabetes when he was two years old, described needing to buy his own insulin once he graduates as “a looming anxiety.”
“On top of being successful to make enough money to afford a home, I also have insulin to worry about,” Bryz-Gornia said. “I don’t have the luxury of being able to take risks. It’s not my fault that I was diagnosed with di- abetes. [Companies found] something to take advantage of. I take the blow.”
Fordham, Grimm and Bryz-Gornia all said they worry about needing to ration insulin at some point.
“When [someone] say[s] they are rationing, they are carefully calculating the food that they are intaking and the activities that they are doing and then providing what they think is going to be the bare minimum of what will be enough,” Fordham said. “It’s guesswork.”
Grimm said after graduating, if she is unable to find a job with good enough insurance to help her cover the costs of her insulin, she sees her two options as having to ration or sacrificing financial well-being to keep herself healthy.
“It’s definitely in the back of my mind, and it will most likely affect how I choose the place that I work after I come out of school,” Grimm said.
Bryz-Gornia said that because insulin is so expensive, he is already taking steps to only use what he needs.
“I take precaution in making sure the insulin stays cold and nothing goes bad,” Bryz-Gornia said. “I only fill my pump half way, which leads to more injections, but I won’t waste anything.”
For now, Fordham said she relies on her parents and their insurance to help her cover the costs of her diabetes. She said she understands the privilege of being able to do so.
“I’m really fortunate that both my parents have great insurance coverage, so I don’t feel it as directly as some other people,” Fordham said. “It is already hard enough being a privileged college student living with this day-to-day. I can’t imagine living vial to vial.”